Medical Malpractice Cases: Real Verdicts, Common Claims, and What Qualifies as Negligence
Medical Malpractice Cases: Real Verdicts, Common Claims, and What Qualifies as Negligence
Nobody expects to walk into a hospital for treatment and leave worse off than they arrived. Yet patients face life-altering complications every day—some from unavoidable risks, others from preventable mistakes. Here's the uncomfortable truth: bad outcomes happen even when doctors do everything right, and determining which injuries deserve compensation requires navigating a complex legal maze most people don't understand until they're thrust into it.
You might assume any medical error automatically entitles you to sue and win. That assumption costs people thousands in wasted legal consultations every year. Courts don't award damages simply because a treatment failed or a diagnosis came late. The law draws careful lines between "my doctor made a mistake" and "my doctor's negligence caused compensable harm."
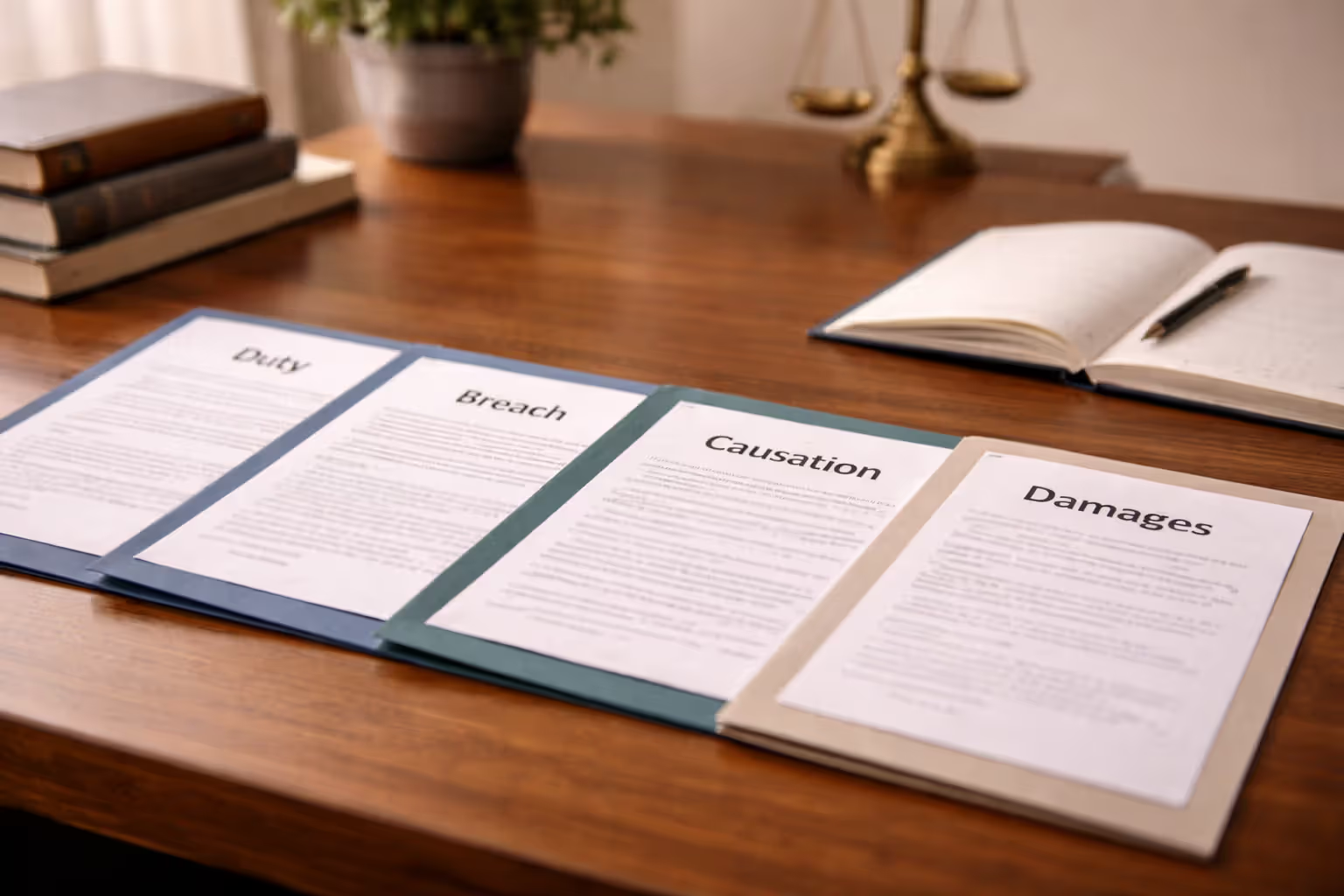
What Legally Defines a Medical Malpractice Case
Proving negligence demands more than pointing at a bad outcome and saying "someone messed up." You'll need to establish four separate legal requirements, and weakness in any single area can sink an otherwise compelling case.
Duty of care confirms that a formal treatment relationship existed. Walk into an ER with chest pain? That creates duty the moment staff begins evaluating you. Ask your neighbor who happens to be a cardiologist about your symptoms at a backyard barbecue? That probably doesn't create duty—informal medical chitchat at social events rarely rises to the level courts recognize as establishing a professional obligation.
Most disputes don't hinge on whether duty existed. Appointment scheduling, hospital admission paperwork, or insurance claim submissions create clear documentation that a treatment relationship formed. Telemedicine visits, phone consultations with your established physician, and covering doctors stepping in for your regular provider all create duty as well.
Breach of standard of care gets complicated fast. You must prove your provider's decisions fell outside what competent peers would have done facing identical circumstances. "Competent" doesn't mean the best doctor in the country—it means reasonable practitioners in similar specialties working with comparable resources.
Medicine is a science of uncertainty and an art of probability.
— William Osler
Consider these variations: A rural ER physician at 2 a.m. with limited diagnostic equipment faces different standards than a specialist at Johns Hopkins with full lab support during business hours. Emergency situations permit decisions that wouldn't pass muster during elective procedures with ample preparation time. The applicable standard shifts based on specialty training, geographic practice patterns, available technology, and time pressure.
Causation requires connecting the breach directly to your injury—and this is where many seemingly strong cases collapse. You can't just demonstrate substandard care; you must prove that specific deviation caused your harm rather than your underlying condition, other health factors, or sheer bad luck.
Here's an example: A surgeon leaves a sponge in your abdomen during gallbladder removal, and you develop a serious infection two weeks later. The causation link is crystal clear—no retained sponge means no infection. Compare that with failing to diagnose lung cancer on an initial X-ray. If expert testimony reveals the tumor had already metastasized throughout your body at the time of the missed reading, proving that earlier detection would have changed your outcome becomes extraordinarily difficult. Maybe earlier chemotherapy extends life by six months. Maybe it makes no difference at all. That ambiguity weakens causation.
Correlation does not imply causation.
— Ronald A. Fisher
Damages means you suffered measurable, quantifiable harm. Medical expenses, lost wages, permanent disability, additional surgeries, ongoing pain requiring treatment—these translate into dollar values courts can award. Emotional distress standing alone, without accompanying physical injury or financial loss, generally doesn't clear the bar for damages.
Let's walk through a scenario that checks all four boxes: A 52-year-old accountant undergoes routine hip replacement surgery. Post-operatively, she develops a severe infection requiring three additional surgeries and eight weeks of IV antibiotics. Investigation reveals operating room staff violated multiple sterile field protocols captured on video—team members reaching across the surgical site without proper technique, dropping instruments on non-sterile surfaces and using them anyway, failing to change gloves after contamination. The patient missed three months of work and now walks with permanent limitations.
Duty? Clearly established through the scheduled surgery. Breach? Video evidence shows flagrant protocol violations, and every surgical expert agrees these deviations are indefensible. Causation? No reasonable explanation exists for the infection besides contamination from observed breaches. Damages? $87,000 in additional medical bills, $42,000 in lost income, plus ongoing pain and permanent mobility restrictions. That case proceeds to settlement or trial with strong prospects for plaintiff victory.
Author: David Kessler;
Source: skeletonkeyorganizing.com
Most Common Types of Healthcare Negligence Lawsuits
Certain error categories dominate malpractice claims. Recognizing these patterns helps you evaluate whether your situation might qualify for legal action or falls into the "unfortunate but not actionable" category.
Surgical Errors and Wrong-Site Procedures
Operating on the wrong body part, leaving surgical tools inside patients, or damaging organs unrelated to the planned procedure generate cases that defendants rarely win. Medicine labels these "never events" because established prevention protocols—verification timeouts, surgical site marking, multiple pre-incision confirmations, mandatory instrument counts—exist specifically to stop them from occurring.
Take wrong-site spine surgery as an example. A patient needs fusion at the L4-L5 level based on MRI findings clearly showing disc herniation and nerve compression at that location. The surgeon operates on L3-L4 instead. The patient now requires a second surgery to address the actual problem, doubling their recovery time and leaving them in worse condition than before the first procedure. Defense teams struggle with these cases because every safeguard failed—the surgical timeout process, the site marking, the imaging review, the intraoperative X-ray verification. One error might get explained away. A cascade of failures indicates systemic negligence.

Author: David Kessler;
Source: skeletonkeyorganizing.com
Nerve damage during surgery presents murkier questions. Orthopedic procedures carry documented risks of nerve injury disclosed during informed consent discussions. Patients sign acknowledgments that certain nerves run near the surgical site and might suffer damage despite perfect technique. Winning these cases requires proving the injury resulted from concrete technical errors—excessive tissue retraction tearing nerve fibers, improper instrument placement cutting structures, failure to identify and protect known anatomical landmarks—rather than an acknowledged risk that materialized despite appropriate care.
Misdiagnosis and Delayed Diagnosis Claims
These cases turn on proving a reasonably competent physician would have reached the correct diagnosis sooner given the same patient presentation, test results, and clinical information. Rare diseases with unusual symptoms make weak cases. Common conditions presenting with textbook findings make strong ones.
Consider a 38-year-old woman who visits her primary care physician three separate times across seven months reporting persistent headaches, progressive vision blurring, and morning vomiting. Her doctor prescribes migraine medication each visit without ordering brain imaging. Eventually, an ER visit for severe symptoms leads to an MRI revealing a sizable brain tumor that's grown substantially during those seven months. Medical experts reviewing the case would likely testify that the symptom pattern—especially the vision changes and morning nausea—screamed for imaging months earlier, and that earlier detection would have enabled less invasive surgery with significantly better outcomes.
Contrast that with a 28-year-old man experiencing occasional chest tightness after large meals. His family physician diagnoses acid reflux and prescribes medication. Eight months later, he suffers a heart attack caused by an undiagnosed congenital coronary artery abnormality. The outcome is tragic, but was the diagnosis negligent? Defense experts might successfully argue that given his age, symptom pattern, absence of cardiac risk factors, and normal initial EKG, reflux represented the most clinically reasonable working diagnosis. Standard protocols don't automatically require cardiac workup for young patients with meal-related chest discomfort and no red-flag symptoms. Without clear evidence that a competent peer would have pursued cardiac testing, the case lacks merit despite the devastating result.
Medication Errors and Pharmacy Mistakes
Wrong medications dispensed, incorrect dosages calculated, failure to check allergy histories or drug interactions, illegible handwritten prescriptions—medication errors cause preventable injuries every day. These cases frequently involve multiple potentially liable parties: the prescribing physician, the dispensing pharmacist, the nurse administering the drug, and sometimes the hospital itself for system failures.
Consider a patient with a documented, highly visible penicillin allergy prominently displayed in their electronic health record. A physician orders amoxicillin (a penicillin-family antibiotic) without checking the allergy list. A pharmacist fills the prescription without catching the contraindication. A nurse administers the dose without verifying allergies. The patient suffers anaphylactic shock causing brain damage from oxygen deprivation. Each professional in that chain bears potential liability—the ordering physician for failing to review allergies, the pharmacist for missing the contraindication check, the nurse for not performing final verification, and possibly the hospital for inadequate fail-safe systems.
Pediatric dosing errors generate particularly catastrophic cases because children require weight-based calculations more prone to mathematical mistakes. A decimal point error—prescribing 10 mg instead of 1.0 mg—delivers a tenfold overdose to a small child. I've seen cases where such errors caused permanent organ damage, neurological injury, or death. The math is simple, the consequences devastating, and the liability clear.
Birth Injuries and Obstetric Malpractice
Labor and delivery complications produce some of the highest-dollar verdicts because injured newborns face 70-80 years of care needs. Failure to perform emergency cesarean sections despite fetal distress, improper vacuum extractor or forceps use, unrecognized maternal hemorrhages, and medication errors during labor dominate these claims.
Fetal heart monitoring creates objective evidence that's hard to dispute. Those continuous tracings show fetal wellbeing in real-time, and concerning patterns—late decelerations after each contraction, loss of heart rate variability, sustained bradycardia—signal oxygen deprivation that can cause permanent brain damage. When monitors display severe distress for 30, 45, or 60 minutes while the obstetric team delays intervention, and the baby is born with cerebral palsy or other neurological injuries, causation becomes easier to establish. Experts can testify that delivery within a specific timeframe would have prevented oxygen deprivation and avoided the injury.
Not every cerebral palsy case succeeds, though. Research shows many instances result from prenatal factors—placental insufficiency, genetic conditions, maternal infections—unrelated to delivery management. Defense teams routinely argue that brain damage occurred before labor even began, making delivery timing irrelevant. These become battle-of-the-experts scenarios where causation remains contested throughout litigation.
Notable Malpractice Verdict Examples from Recent Years
Examining real case outcomes reveals the dramatic range of results in medical error litigation. Award amounts swing wildly based on injury severity, how sympathetic jurors find each side, state damage caps, and whether the evidence clearly demonstrates negligence or requires nuanced medical judgment calls.
| Case Type | State | Year | Verdict/Settlement | Key Facts | Outcome |
| Wrong limb amputation | Florida | 2019 | $12.5M jury award | Diabetic patient's healthy leg amputated; diseased leg still required removal afterward | Jury favored plaintiff; Florida's statutory cap reduced final payment to $8M |
| Missed myocardial infarction | California | 2020 | $4.2M jury award | Emergency physician sent 52-year-old woman home with anxiety diagnosis; cardiac arrest caused death six hours later | Plaintiff verdict; parties reached undisclosed settlement amount during appeals process |
| Cerebral palsy birth injury | Pennsylvania | 2021 | $41.5M jury award | Obstetric team delayed emergency cesarean 90 minutes despite sustained fetal distress signals | Plaintiff secured verdict; ranks among Pennsylvania's largest obstetric malpractice awards |
| Colonoscopy anesthesia mishap | Texas | 2018 | $2.8M settlement | Intubation performed incorrectly during routine procedure caused permanent brain damage | Settled before trial; confidentiality agreement prevents disclosure of settlement structure |
| Retained surgical sponge | New York | 2020 | $3.1M jury award | Sponge remained in abdomen after hysterectomy causing sepsis and requiring emergency bowel resection | Hospital conceded liability; jury trial determined only damage amounts |
| Overlooked lung cancer | Illinois | 2019 | Defense verdict | Radiologist didn't note small nodule on chest X-ray; malignancy found 18 months later | Defense won; testimony established cancer had already spread extensively when first imaging occurred |
| Pharmacy overdose death | Georgia | 2021 | $7.9M jury award | Major pharmacy chain dispensed ten times prescribed blood thinner dose; patient died from brain hemorrhage | Plaintiff verdict against corporate pharmacy defendant |
| Paralysis after spinal fusion | Ohio | 2020 | $15.2M jury award | Neurosurgeon caused spinal cord damage during fusion procedure | Plaintiff won; even defendant's own expert witness acknowledged surgical technique problems |
Notice the pattern? Clear-cut errors—operating on wrong body parts, leaving foreign objects inside patients, extreme delays responding to obvious emergencies—produce plaintiff victories. Cases requiring subtle medical judgment calls, weighing diagnostic possibilities, or evaluating whether standards were met generate more defense wins. Injury severity directly drives verdict size: permanent disabilities and deaths command far higher compensation than temporary complications with full recovery.
How Courts Determine Doctor Liability in Medical Error Litigation
Establishing legal liability requires more than showing an injury occurred or that alternative approaches might have worked better. The legal framework demands specific evidence that the healthcare provider's conduct fell below professionally accepted standards.
Standard of care testimony must come from qualified medical experts—you can't simply argue your position and expect jurors to decide. A plaintiff needs credentialed physicians (typically in the same medical specialty as the defendant) willing to testify that the treatment deviated from what competent practitioners would have done under similar circumstances. This expert requirement protects physicians from hindsight bias and ensures evaluation by professional peers rather than medically unsophisticated jurors making gut decisions.
Qualifying experts must demonstrate current knowledge of medical literature, treatment guidelines, and practices in comparable clinical settings. Courts won't let an academic medical center subspecialist impose university hospital standards on a solo rural practitioner with limited resources and consultant access. Acceptable practice patterns vary based on setting and available support, though this geographic distinction has narrowed as telemedicine, electronic medical records, and internet-accessible clinical resources standardize information availability nationwide.
Comparative negligence (also called comparative fault) reduces plaintiff awards when their own actions contributed to injury. Suppose a diabetic patient repeatedly ignores physician warnings about daily foot inspections and proper wound care. They develop a foot ulcer that progresses to severe infection requiring below-knee amputation. If the jury determines the patient bears 40% responsibility for ignoring clear medical advice and the physician bears 60% responsibility for delayed infection treatment, a $1.5 million verdict gets reduced to $900,000 (the plaintiff's 60% share).
Comparative negligence systems vary by state. "Modified comparative negligence" bars any recovery if plaintiffs exceed 50% or 51% fault (depending on the state). "Pure comparative negligence" reduces awards proportionally even if plaintiffs bear primary responsibility. A plaintiff 80% at fault in a pure system still recovers 20% of damages; the same plaintiff in a modified system recovers nothing.

Author: David Kessler;
Source: skeletonkeyorganizing.com
Tort reform damage caps limit non-economic damages (pain, suffering, emotional distress, loss of life enjoyment) in numerous states. California's cap sits at $250,000—a figure unchanged since 1975 despite inflation. Texas restricts non-economic damages to $250,000 per physician defendant and $500,000 total per case regardless of how many defendants share liability. Economic damages—medical expenses, lost income, future care costs, therapy needs—face no caps in most jurisdictions.
These caps dramatically reshape case values, particularly affecting young patients and retirees who lack substantial wage loss to claim. Picture a 23-year-old left paraplegic by surgical error. Future care costs might total $12 million over his life expectancy (economic damages flow unrestricted). But profound suffering, loss of mobility, inability to participate in activities he enjoyed, sexual dysfunction, and loss of life pleasure gets capped at $250,000 in California despite representing the most significant impact on his existence. That identical case in New York or Pennsylvania with no non-economic caps might secure $5-8 million for those non-economic harms.
Res ipsa loquitur (Latin for "the thing speaks for itself") occasionally allows plaintiffs to sidestep detailed standard-of-care testimony when injuries couldn't possibly occur without negligence. Surgical instruments remaining inside patients after procedures or operations performed on wrong body parts invoke this doctrine. The injury's mere existence proves negligence, shifting burden to defendants to explain how it happened despite reasonable care—an explanation that rarely exists for such events.
Settlement vs. Trial: How Most Cases Actually Resolve
Somewhere between 90-95% of filed medical malpractice lawsuits settle before reaching trial. Understanding why cases settle versus proceeding to verdict helps set realistic expectations if you're considering pursuing a claim.
Settlement incentives include certainty, faster resolution, and cost control. Trials consume three to five years and hundreds of thousands in expert witness fees, deposition expenses, and legal costs. A $650,000 settlement offer in year two might exceed the realistic expected value of pursuing trial three years later when you factor in verdict uncertainty, additional appeal delays, and mounting expenses draining any award.
Defendants avoid public trials that generate negative publicity, detailed testimony about errors, and risk of punitive damages. Physicians dread taking the witness stand to discuss mistakes, and hospitals prefer confidential settlements to public verdicts that might encourage additional claims from other patients. Medical malpractice insurers run cold calculations: paying $800,000 to settle today costs less than spending $175,000 preparing for trial while risking a $2.5 million jury verdict.
Plaintiffs accept settlements to eliminate trial stress, guarantee recovery for injured family members, and avoid verdict uncertainty. Juries can be wildly unpredictable—they might award nothing, or far less than claimed damages. A plaintiff facing $400,000 in medical bills and permanent limitations might accept a $750,000 settlement rather than risk a defense verdict leaving them with nothing and owing their attorney for advanced costs.
Cases proceeding to trial typically involve significant disagreement about whether negligence occurred or what damages should be. When defendants maintain they provided appropriate care within standards and plaintiffs insist on clear negligence, neither side perceives enough settlement value to bridge the gap. Catastrophic injuries with lifetime care needs also resist settlement because the chasm between what plaintiffs demand ($15-40 million) and what defendants offer ($1-4 million) proves too wide to cross.
Some plaintiffs refuse settlement seeking vindication or accountability beyond money. A patient believing a surgeon's pattern of errors endangered others may insist on public trial despite reasonable settlement offers. Some want their day in court—a chance to confront the provider, tell their story publicly, and force acknowledgment of wrongdoing that confidential settlements prevent.
Timeline expectations vary enormously by court location. Fast-track jurisdictions like Texas and Florida push cases to trial within 18-30 months of filing. Congested courts in New York or California might take four to six years reaching trial. Discovery—exchanging medical records and documents, deposing witnesses, retaining and preparing expert witnesses, filing motions—consumes the vast majority of this time. The actual trial typically lasts one to three weeks depending on case complexity.
Settlements cluster around litigation milestones. Many cases settle immediately after depositions reveal damaging testimony or after expert reports clearly establish liability. Defense settlement offers often increase substantially once trial dates approach and mounting defense costs create urgency. I've seen cases settle during jury selection or even mid-trial when parties reassess their positions after watching witness testimony.
Statute of Limitations and Filing Deadlines by State
Missing filing deadlines destroys otherwise valid claims worth millions. Each state imposes strict timeframes for initiating lawsuits, with only narrow exceptions that don't help most injured patients.
Standard limitations periods typically range from one to three years measured from when injury occurred or when you discovered the harm. These deadlines balance your need for recovery time and investigation against defendants' interest in resolving potential claims while evidence remains fresh, witnesses' memories stay accurate, and medical records still exist.
The discovery rule extends deadlines when injuries weren't immediately apparent at the time they occurred. A surgical sponge remaining in your abdomen might not trigger symptoms for months or years after surgery. Most states start the clock when you discovered or reasonably should have discovered the injury occurred, not when the negligent act happened. "Should have discovered" creates disputes—defendants argue symptoms should have prompted earlier investigation while plaintiffs contend nothing suggested a retained object until specific complications arose.
Statutes of repose impose absolute deadlines regardless of when discovery occurred. A state might allow two years from discovery but never permit filing more than five years after the negligent act. These provisions prevent claims filed decades after incidents based on recently discovered connections between old treatment and current problems.
| State | Standard Deadline | Discovery Rule? | Absolute Cutoff | Notable Exceptions |
| California | Three years from incident OR one year after discovery | Applies | None specified | Requires 90-day advance notice before filing suit |
| Texas | Two years from incident or from discovery | Applies | Ten-year maximum | Must file expert report supporting claims within 120 days of filing |
| Florida | Two years from discovery | Applies | Four years from incident (with narrow exceptions) | Fraud or intentional concealment extends all deadlines |
| New York | Two and one-half years from incident | Very limited application | Ten years for retained foreign objects | Continuous treatment by same provider may extend deadline |
| Pennsylvania | Two years from incident | Applies | Seven-year maximum | Minors have until their 20th birthday to file |
| Illinois | Two years from discovery date | Applies | Four years from incident | Minors and fraudulent concealment create exceptions |
| Ohio | One year from discovery OR from incident | Applies | Four-year maximum | Among shortest deadlines; immediate action required |
| Georgia | Two years from incident | Limited application | Five-year maximum | Retained foreign objects have no repose limitation |
| Michigan | Two years from discovery OR six months after ending care | Applies | No repose limit | Continuous treatment relationship extends filing deadline |
| North Carolina | Three years from incident | Very limited | Four-year maximum | Foreign objects and fraudulent concealment excepted |
| Arizona | Two years from incident or discovery | Applies | No repose limit | Notice of claim to provider required before filing |
| Massachusetts | Three years from discovery | Applies | Seven years from incident | Minors under six have until ninth birthday |
| Washington | Three years from incident OR one year from discovery | Applies | Eight-year maximum | Must notify healthcare provider 90 days before filing lawsuit |
| Tennessee | One year from incident | Very limited application | Three-year maximum | Extremely short deadline demands immediate consultation |
| Maryland | Five years from incident OR three years from discovery | Applies | None (with exceptions) | Longer deadline offset by complex procedural rules |
Minor patient exceptions exist throughout most states. Children typically receive extended deadlines, often allowing claims until reaching age 18 plus the standard limitations period. Some states pause (or "toll") deadlines for mentally incapacitated patients unable to pursue claims during their incapacity.

Author: David Kessler;
Source: skeletonkeyorganizing.com
Fraudulent concealment by healthcare providers—actively hiding errors, falsifying medical records, lying about injury causes—extends deadlines in many states. A surgeon who deliberately alters operative notes to cover up a mistake might face claims filed years later once the deception gets discovered through subsequent treatment or independent record review.
Consulting an attorney immediately after suspecting malpractice remains absolutely critical. Pre-filing requirements—formal notice letters, expert affidavits establishing merit, medical review panel evaluations—consume months before lawsuits can even be filed. Waiting until approaching the deadline makes timely filing impossible once you account for these mandatory preliminary steps.
Frequently Asked Questions About Medical Malpractice Claims
Evaluating potential medical malpractice claims demands understanding both legal requirements and medical realities. Plenty of bad outcomes don't qualify as negligence, and not every instance of negligence justifies the enormous expense, time investment, and emotional stress litigation demands. All four required elements—duty, breach, causation, and substantial damages—must coexist, and the damages must be significant enough to justify pursuit once you factor in costs potentially exceeding $150,000.
Time-sensitive deadlines make immediate action essential. Waiting months to consult attorneys risks missing filing deadlines or losing critical evidence forever. Medical records face destruction after retention periods expire, witnesses' memories fade and become less useful, and statutes of limitations run out without exceptions. Anyone suspecting negligence should request complete medical records immediately and consult experienced attorneys within weeks—not months or years later.
The gap between filing a lawsuit and final resolution typically spans two to five years depending on jurisdiction and case complexity. Settlement negotiations, expert witness depositions, motion practice, and trial preparation consume time and emotional energy most people underestimate. Developing realistic expectations about probable timelines, likely outcomes based on similar cases, and reasonable financial recovery ranges helps patients make informed decisions about whether pursuing claims makes sense or whether focusing energy on physical recovery and moving forward serves them better.
Related Stories

Read more

Read more

The content on skeletonkeyorganizing.com is provided for general informational and inspirational purposes only. It is intended to showcase fashion trends, style ideas, and curated collections, and should not be considered professional fashion, styling, or personal consulting advice.
All information, images, and style recommendations presented on this website are for general inspiration only. Individual style preferences, body types, and fashion needs may vary, and results may differ from person to person.
Skeletonkeyorganizing.com is not responsible for any errors or omissions, or for actions taken based on the information, trends, or styling suggestions presented on this website.